Pump Fit Matters
/Getting a good pump fit is vital, especially when you pump often and the breast-pump part your nipple is drawn into (the nipple tunnel) is composed of rigid plastic, as is true of most pumps. If it is made of soft silicone, which a few pumps are, it may mold more easily to different nipple sizes.
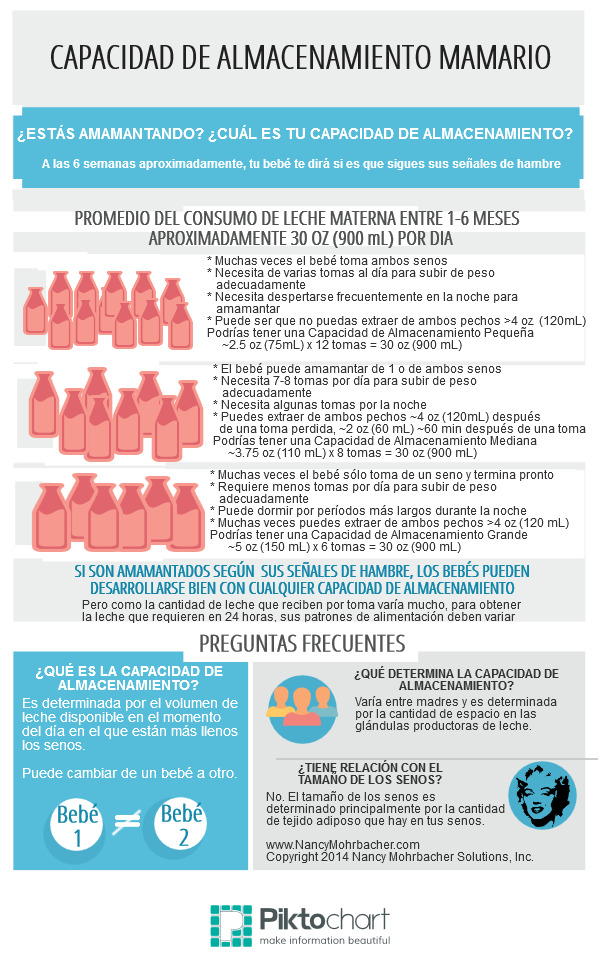
Figure 1
Pump fit affects both nipple comfort and milk flow. When a nipple tunnel is too small, it can lead to pain, skin trauma, and reduced milk flow, because it compresses the nipple during pumping. In pump-dependent families, this can put milk production at risk.
Pump Fit and Nipple Diameter
Pump fit is based on how well your nipples fit into the pump’s nipple tunnel. Pump manufacturers call the pump part with the nipple tunnel by different names (flange, shield, breastshield). Some parents refer to it as the “horn” or “funnel.”
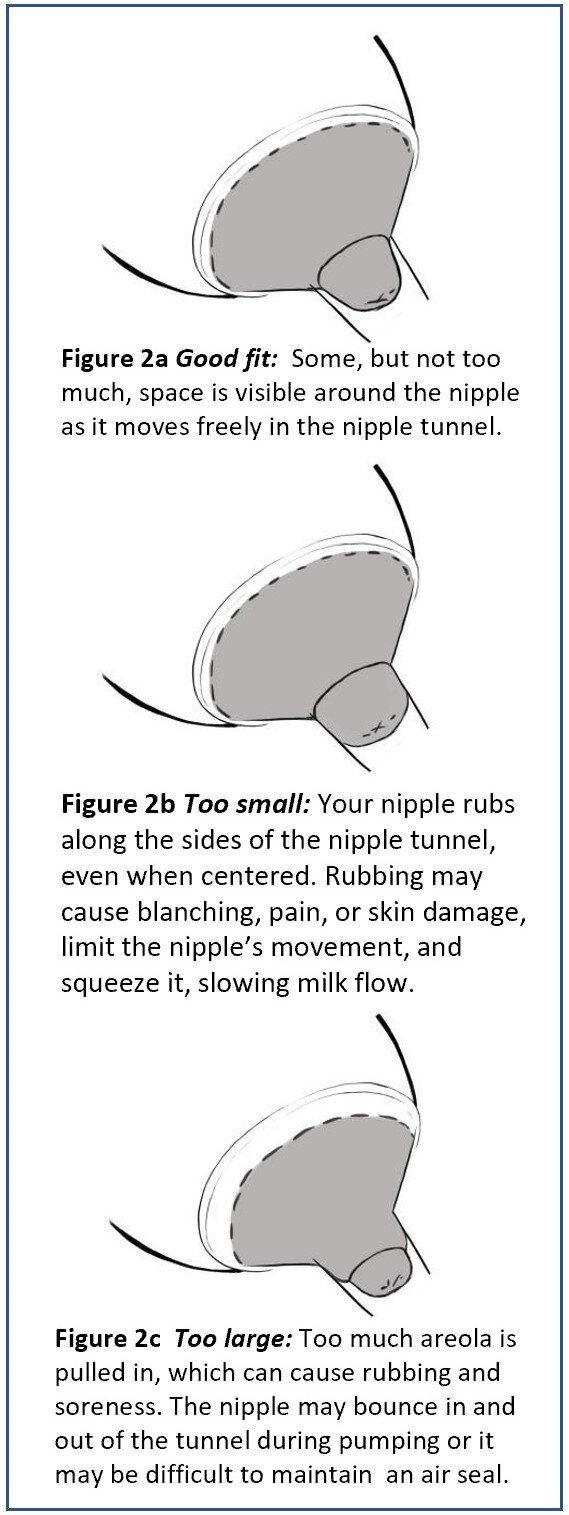
Figure 2
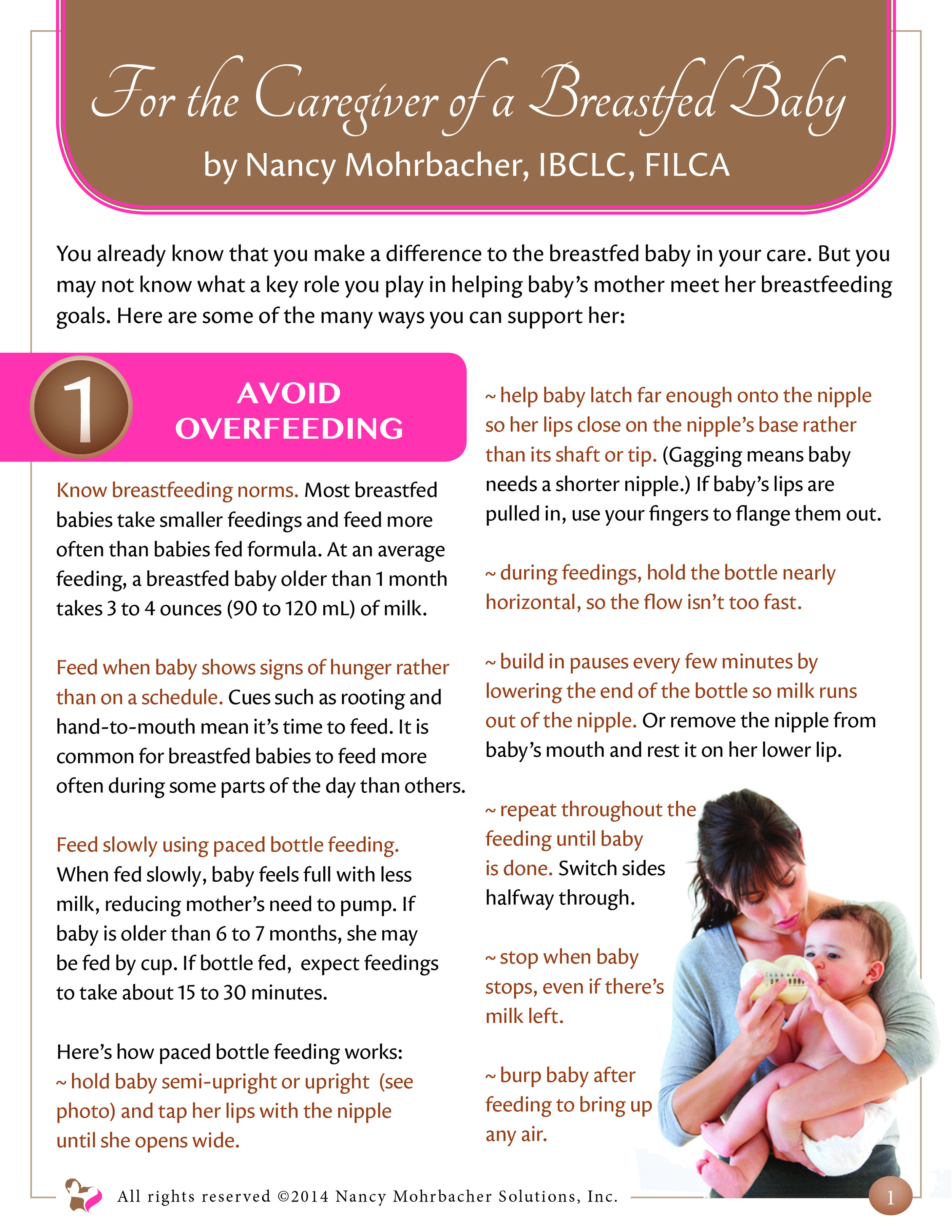
Nipple tunnel diameter varies slightly by brand (Figure 1), with 24 or 25 mm the standard diameter of most pumps. One sign a different size nipple tunnel is needed is pain or discomfort during pumping, even near the pump’s lowest suction setting. Because the left and right nipples may vary in size, some parents get the best results when they use one size on one side and another size on the other side.
If pumping is comfortable with good milk flow, you probably have a good pump fit. If there is discomfort, even on low suction settings, watch your nipples during a pump session and see how they compare with Figures 2a, 2b, and 2c.
Depending on the pump brand, larger or smaller nipple tunnels may be available for purchase separately.
How Often Are Larger or Smaller Nipple Tunnels Needed?
More often than you might think. In one U.K. study, 36 mothers with babies in the NICU pumped with a standard 25 mm nipple tunnel, and the researchers noted that because they reported discomfort, the opening was too small for 28%. The authors wrote: “If the [opening] is too small, pressure is highest on the nipple tissue, which can cause sore nipples and ineffective drainage.”2
In a U.S. NICU study, a different brand of pump with a 24 mm standard nipple tunnel was used. When both milk flow and comfort were assessed, a much higher percentage of mothers had better results with a larger diameter nipple tunnel. “[W]e found that 51.4%—or about half—of the 35 mothers who served as subjects in the research initially required either the 27 or 30 mm shield in order to achieve optimal, pain-free nipple and areolar movement during milk expression. As lactation progressed, 77.1%—or slightly more than three quarters—of the mothers eventually found they needed these larger shields.”3
Pump Fit Can Change with Regular Pumping.
A 2019 U.S. randomized crossover study compared the effects of nursing, hand expression and pumping on the nipple sizes of 46 lactating women1. The researchers found that unlike direct nursing and hand expression, with pumping, nipple length and diameter increased in size. Two U.S. lactation consultants used an engineer’s template to measure mothers’ nipples before and after pumping and also found that pumping causes nipples to increase in size. They wrote: “Pre- and post-pumping measurements taken with a circle template reveal that nipple size can increase 3 to 4 millimeters.”4 So even if parents are fitted well when they start pumping, it makes sense for them to check their pump fit over time to see if it has changed and whether they need a larger diameter nipple tunnel.
Signs a Larger or Smaller Nipple Tunnel Is Needed
Consider a larger nipple tunnel if:
• You feel discomfort, even on low suction settings.
• Your nipple rubs along the tunnel, despite efforts to center it.
• Your nipple blanches, or turns white.
• Your nipple does not move freely in the nipple tunnel.
• You notice slow milk flow or less milk expressed than expected.
Consider a smaller nipple tunnel if:
• You feel discomfort, even on low suction settings.
• More than about 1/8 inch (3 mm) of the areola is pulled into the nipple tunnel.
• Your nipple bounces in and out of the tunnel.
• You have difficulty maintaining an air seal.
Major breast-pump brands, such as Ameda, Medela, and Spectra offer fit options ranging from 20 mm to 36 mm. Another product that can sometimes help make pumping more comfortable is Pumpin’ Pal, which provides an angled nipple tunnel. Contact a lactation supporter for help in finding the best fit for you. See also the blog post HERE for other reasons pumping might feel uncomfortable.
References
1 Francis, J., & Dickton, D. (2019). Physical analysis of the breast after direct breastfeeding compared with hand or pump expression: A randomized clinical trial. Breastfeeding Medicine, 14(10), 705-711.
2 Jones, E., Dimmock, P. W., & Spencer, S. A. (2001). A randomised controlled trial to compare methods of milk expression after preterm delivery. Archives of Disease in Childhood. Fetal and Neonatal Edition, 85(2), p. F94.
3 Meier, P. (2004). Choosing a correctly-fitted breastshield. Medela Messenger, 21, p. 8.
4 Wilson-Clay, B., & Hoover, K. (2017). The Breastfeeding Atlas (6th ed.). Manchaca, TX: LactNews Press, p. 80-81.